Kushal Suryamohan (PhD), Bioinformatics Scientist, MedGenome (USA)
Snake Genomics
For the majority of people, the mere mention of snakes conjures involuntary shivers! These stealthy critters have a forked tongue, unblinking eyes and either have fangs that deliver venom to immobilize/kill prey or strong muscles to asphyxiate. Snakes have been around for millions of years, and have used this time to become incredibly effective predators and can be found on all continents except Antarctica. Beginning over a 100 million years ago, snakes diverged from lizards, lost their legs and evolved into smaller and faster hunters to catch quick-moving prey. Rather than expend a great deal of energy to forage for food, many snakes developed venom – a complex chemical cocktail of proteins and enzymes designed to kill or incapacitate the prey even before ingesting their meals. The toxins in these venoms have been refined over millions of years to target highly specific pathways that affect their prey’s vital bodily functions. Some toxins are neurotoxins while some disrupt hemostasis and several others that are cytotoxic. Some snakes are so dangerous that people die from such encounters. According to the most recent report by the World Health Organization, about 5 million people are bitten by snakes and ~100,000 are killed annually.
There are more than 3000 identified species of snakes, of which over 600 are known to be venomous. India, where snakes are both feared and worshipped as mythological animals, has roughly 300 snake species, of which ~60 are venomous. Given that most of India’s population still lives in rural areas, encounters with snakes are quite frequent with > 45,000 snakebite-related deaths every year and these are only estimates as incidences of snakebites are often underreported. The “big four” snakes of India – the spectacled cobra, common krait, Russell’s viper and saw-scaled viper cause the most fatalities.
While antivenom, the only currently approved form of treatment for snakebites, is freely available in public hospitals, there are several issues with the current practices in antivenom manufacturing, often resulting in anti-venom that is poorly efficacious. One reason for this is snake venom and its potency differs between species, and even between snakes of the same species between regions. For instance, while doctors have been known to administer 2-3 vials of a certain antivenom against a species of snake in one part of India, more than 25 vials of the same serum are required to treat a victim bitten by the same snake in another part of the country. Another reason for this lack of efficacy is the archaic technology used for antivenom manufacture. Antivenom manufacturers still use a technology that was first pioneered ~120 years ago (about 30 years before penicillin was discovered by Alexander Fleming). This method relies on the use of snakes for milking their venom glands to extract venom. Small amounts of venom are then repeatedly injected into horses to create an immune response. Antibodies are then extracted from the blood and packaged as antivenom (with a few minor steps in between that help extend the antivenom shelf life). Needless to say, this is a laborious and expensive process. More importantly, over 70% of the antibodies in this antivenom cocktail do not target the toxins that cause the most damage in snakebite victims. This is because when antibodies are extracted from the horse’s blood, you do not only find those that recognize the snake toxins but also countless other antibodies are recovered which have no therapeutic effect on the snakebite as these antibodies recognize bacteria, viruses, hay, dust, and other environmental stimuli the horse may have been exposed to. Therefore, such antivenoms are typically less potent and necessitate administration of multiple doses of antivenom per treatment. Another consequence of this is that the antivenom can cause adverse reactions in the patient/victim including hyperallergic reactions such as serum sickness, kidney failure and anaphylactic shock, which can kill the snakebite victim if the snake does not do so first. Another critical drawback is the poor efficacy of such antivenoms – many snake venom toxins are small proteins and are poorly immunogenic and therefore are not attacked by the horse’s immune system.
Given these drawbacks, several alternative antivenom manufacturing methods have been proposed. One such approach that has gained increasing attention is the use of phage display technology. Phage display technology is a high-throughput approach to discover human antibodies specific to different antigens. Several antibodies discovered using phage display technology have been approved for use as drugs to treat a number of human diseases, ranging from cancers to autoimmune disorders. Using this approach, it is now feasible to develop humanized antibodies that can target key proteins, like potent toxins, to create effective and safe antivenom. In lieu of relying on snakes for venom, knowledge of the toxins and their genomic coding sequences for a given species will instead allow for the synthesis and expression of venom components using recombinant DNA technology. These can then be used as antigens for antibody discovery. A cocktail of such antibodies against the most potent toxins can be combined to yield a synthetic antivenom of a defined composition. Importantly, these humanized antibodies will not elicit an immune response from patients and can be produced using standard lab approaches for drug manufacture. Equally important, this approach will lead to a more humane and cost-affordable approach to antivenom manufacture as it does not require maintaining a collection of snakes for venom extraction or horses for antivenom development.
While the above mentioned methods are superior for antivenom development, large animal-based antivenom production, using extracted snake venoms, still continues to be the standard practice. This is due to several factors including socio-economic barriers, low funding for research initiatives, the complexity of developing an alternative treatment, and low economic incentives for pharmaceutical companies to develop antivenoms. In 2018, snakebite envenoming was added to the World Health Organization’s (WHO) list of Category ‘A’ Neglected Tropical Diseases in 2017, thereby bringing renewed attention and focus on promoting research and development efforts into novel snakebite antivenom therapies.
A significant hurdle in developing nextgen antivenom is the gap in our understanding of snake venom. Much of our current knowledge on snake venoms is based on proteomic studies and they have provided an incomplete picture of the venom components. Mass spectrometry of venom relies on a good database of proteins to accurately identify the constituent components. Given the limited genomic or transcriptomic reference datasets for venomous snakes, this database of venom proteins is not comprehensive.
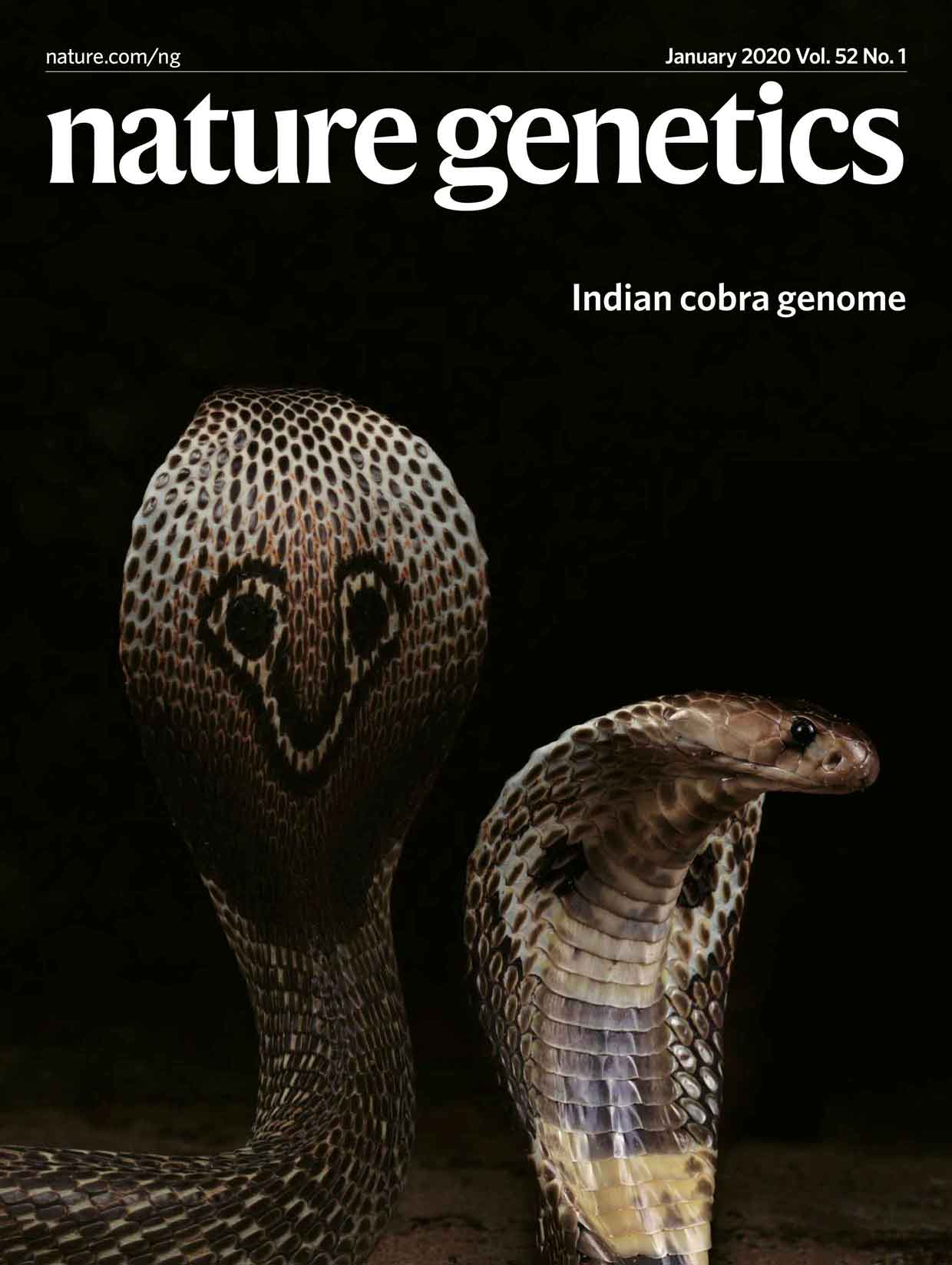
Our impetus to get involved in snakebite and antivenom research was fueled by this gap in antivenom manufacture technology. Given MedGenome’s expertise in the NGS space, we leveraged this experience and utilized several genomics sequencing technologies including long-read, short-read sequencing platforms, optical mapping and chromosome conformation capture methods to produce the first high-quality reference genome of the Indian cobra. This study was recently published in Nature Genetics and was featured on the cover of the January 2020 issue. Besides the genome, we also published a comprehensive catalogue of venom genes for this medically important snake. An integrated analysis of genome, transcriptome and venom proteome of the Indian cobra revealed 12,346 genes that were expressed in the venom gland that included 139 toxin genes from 33 different toxin families. From this list, we identified 19 genes that were primarily expressed in the venom gland. Using proteomic data from the venom, we confirmed the presence of 16 of these toxins. It is likely that these toxins form the major components of this species’ venom and targeting these venom-specific toxins using synthetic antibodies should neutralize the major toxic effects. This information can be used for rational design and expression of toxins of interest using recombinant DNA technology. Recombinantly produced toxins can then be used for developing synthetic antibodies using phage display technology. Once identified and tested, the resulting synthetic human antibodies against the different toxins can be produced on a large scale and combined to yield a safe and effective antivenom. We envision such an antivenom can be manufactured in a cost-effective manner and be made more accessible across India. This approach will modernize antivenom development and set the stage for the generation of a broad spectrum antivenom against the ‘Big Four’ Indian snakes.
Our study has given insights into previously unknown genetic structure and variations in venom genes within a given snake species. This study provides a useful genomic resource which will facilitate studies of venom biology, evolution, drug discovery and antivenom research in Asia and across the world.
Another aspect of our venture into snakes is the fact that despite their deadly nature, venom is one of nature’s most beautifulparadoxes. By design, venom is meant to kill, and it does this job frighteningly quickly and efficiently! Yet, the same properties that make it deadly can also be harnessed to provide potent healing. Several components of venom often target the same molecules that medicines target to treat diseases. Indeed, out of the ~1,000 venom toxins that have been analyzed by scientists so far, about a dozen drugs have been developed and brought to market. There are already six drugs approved for use by the FDA (Food and Drug Administration) in the USA – all derived from venom. To date, the FDA has approved seven drugs derived from animal venom for conditions such as high blood pressure, heart conditions, chronic pain, and diabetes. Ten more are currently in clinical trials while many others are in pre-trial stages. And we have only barely scratched the surface – with an estimated 300,000 venomous animals found across the world and ~50-60 unique toxins in each species, there are ~20 million potential toxins, each with its own targets and effects that remain unexplored. While snakes are our primary species of interest for venom research, we are also studying other venomous creatures, from venomous caterpillars to jellyfishes, centipedes, scorpions and many more. Our goal is to catalogue the genomes and venom of these species and thus create a rich resource for drug discovery. Stay tuned for more updates on the fascinating world of venomous animals.
References:
- Suryamohan K., et al, The Indian cobra reference genome and transcriptome enables comprehensive identification of venom toxins. Nat Genet 52, 106–117 (2020).
- World Health Organization snakebite resource – https://www.who.int/health-topics/snakebite
- Gutiérrez, J., Calvete, J., Habib, A. et al. Snakebite envenoming. Nat Rev Dis Primers 3, 17063 (2017).
- Venoms to Drugs: Venom as a Source for the Development of Human Therapeutics. Ed. By Glenn F. King (https://doi.org/10.1039/9781849737876)
- Phage display technology – George P. Smith* and and Valery A. Petrenko, Chemical Reviews 1997 97 (2), 391-410
#Snake Genomics, #human antibodies, #DNA technology, #antibody discovery
 US
US IN
IN